Centre for Vision, Speech and Signal Processing (CVSSP)
Creating machines that can see and hear to understand the world around them.
Our Centre is an internationally recognised leader in audio-visual machine perception research. With a diverse community of more than 150 researchers, we are one of the largest audio and vision research groups in the UK.
Research in the Centre has led to award-winning spin-out companies in the biometric, communication, medical and creative industries.

Join our renowned Surrey Institute for People-Centred AI (PAI)
The pan-University PAI at the University of Surrey offers a unique environment to help shape the future of AI as part of a community of co-creators.
Can machines think?
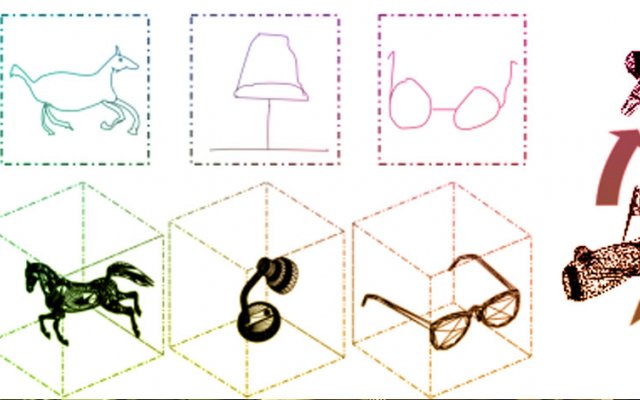
Over the past thirty years, we have become an international centre of excellence for training and research in audio and visual machine perception in collaboration with industry. Our research has pioneered new technologies for the benefit of society and the economy, with applications spanning healthcare, security, entertainment, robotics, autonomous vehicles, communication and audio-visual data analysis.
Today we again ask the question: Can machines think?
Research highlights
Learn more about our research from the CVSSP digital book and our YouTube channel.
Making major contributions
Our Director, Professor Adrian Hilton, was awarded the Institute of Engineering and Technology Achievement Medal for major and distinguished contribution to computer vision engineering.
What we have to offer
We advance research in artificial intelligence (AI) and machine perception structured in seven labs focused on cross-disciplinary application areas and are always looking for businesses to collaborate with us.
Take a look at our staff opportunities to see what roles are currently vacant.
Study with us
Our postgraduate research community is internationally diverse with students of all ages studying on a full or part-time basis.
Upcoming events
Stay connected
Latest tweets
@cvssp_research



Latest blog posts
Protected: The Future says AI. Are we ready?
There is no excerpt because this is a protected post.